Managed care oversight and work products: Service Coordination, Clinical Oversight, and Network Adequacy (also starting administrative simplification, and outcome-based performance management). Juliet Sharon and team (Staff). There are six initiatives in play at the moment that started over the past year.
Network Adequacy
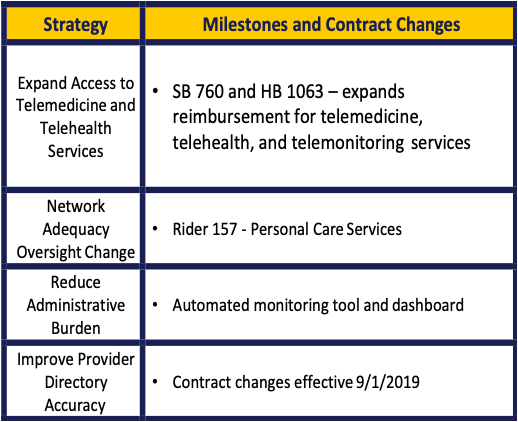
There are also rate issues and access-to-care issues outside of managed care. Policy guidance will be provided to MCOs related to telemedicine, associated costs, and offsetting value. Telemedicine providers would be required to send back information about the service to the primary care provider.
There are 34 different provider types that are monitored at this time. There is a network adequacy requirement for personal care services and choice. Other alternatives are also required to be provided.
Regarding the reducing administrative burden, data is collected, and studies are being conducted. They are trying to pull all the information into a performance dashboard and hope to have an automated system for processes that are currently done manually.
Provider Directory will be included into a master file that will have all the providers in the managed care network. They are striving to have the MCOs correct incorrect data in the directories.
Ms. Murphree stated that CFC and non-CFC should be included. Staff stated that all the services provided through Managed Care are included as well as fee-for-service.
Ms. Rummel stated that the health plans will be matching directory information with the master file. They have found that the master file is often incorrect. Will that be updated? Staff stated that it will be and that providers should update their information, but often only update with the MCO and not the master file. HHSC is working on getting two-way information to keep both provider files and master files current. Ms. Rummel stated that it would be helpful to have an automatic feed to the master file.
A member stated that psychiatry is a huge void and asked if this is a focus. Staff stated that there is a statewide access issue with psychiatry. They do monitor psychiatry and pediatric subspecialties. Most services provided through telehealth and telemedicine are behavioral health services.
The Vice Chair stated that the access-related information has been an issue. Staff stated that there is a Complaints Workgroup targeting the different complaints categories. Complaints data will be integrated with the performance dashboard. The Vice Chair stated that if the data is not maintained, the complaints stop coming forward. Staff stated that there are a lot of data issues and data flow issues.
Clinical Oversight
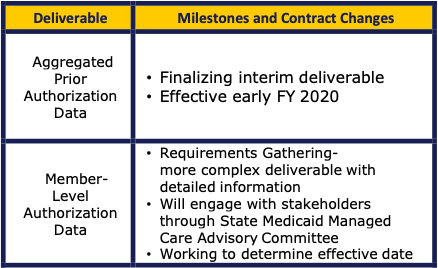
The highest priority deliverables under clinical oversight are presented above. The member level is really at the individual PA request level. Funding was recently received from the legislature to clean the data. They are looking at an effective date of the end of 2020.
Ms. Rummel clarified that the goal was to watch timeframes and inquired about the goals. Staff stated they are looking for outliers in the process.
Ms. Murphree inquired about the outliers. Staff stated that outliers are not at one point in time. They are also at the service management level and they want to be able to course correct within the managed care plan.
The Vice Chair stated that it is not to identify extreme utilization by an individual. Staff stated they collect that data and they are looking at issues across health plans as well.
Mr. Piccola stated that full denials and partial denials should be included. Staff stated that partial and administrative denials have to be reviewed also. They are thinking about how they are overseeing that, and the new data process should help.
Service and Care Coordination
The above includes all managed care programs across the four domains listed above. They are establishing consistent terminology across all programs. They also want to align and clarify MCO expectations. HHSC wants to better communicate definitions of terms and what is intended for service coordination.
Regarding oversight, they did an assessment across HHSC. There are functions at different levels. They are reviewing the onsite processes and increasing use of a new deliverable for service coordination, working with stakeholders and MCOs to implement this domain.
Enhancing coordination is trying to look at the different waivers and the MCO service coordination. They are working to identify where the gaps may be and will be providing technical assistance.
They have reviewed other state’s implementation of best practices (NY, FL, AZ, TN, LA, WA).
Dr. Collins stated that there will often be a LIDDA and MCO service coordinator and asked if the coordination will look across these different coordinators. Staff stated that they are looking at critical elements at MCOs and requiring consistent use of terminology in the MCO contracts. Once the website is up, it will help clarify.
Ms. Caruso commented on enhanced community coordination and the brand-new service of habilitation coordination. These have different caps for caseloads. Will the contract amendment put caseload maximums on MCOs? Staff stated that at this time, that is not planned. HHSC does onsite reviews and the team is looking at the coordination tool for when they go onsite, and the service coordination models and staffing models for service coordination. Concern was expressed regarding the more vulnerable populations and coordination needs.
Ms. Lawler stated that tightening up language is important, but so is understanding the required functions. Different caseload sizes often speak to the different functions being performed. It is not that one case manager function is better than the other but that they are different from one another.
Ms. Lawler asked what the assessment might look like. Staff stated that they are working with subject matter experts and they are looking at the different touchpoints. Subject matter expertise is being accessed from HHSC.
Ms. Rummel stated that it would be great to have clarity from the health plan side and program inconsistencies. There may be misunderstanding from providers. There are also inconsistencies from different IDD programs (including the fee-for-service side). She stated that clarity is something all agree is needed.
Ms. Smith inquired what the plans were for stakeholder input. Staff stated that for all the initiatives, the state Medicaid Managed Care Advisory Committee has been identified as the hub along with the development of subcommittees. As these are established, more information can be provided. That will be one venue for stakeholder feedback and HHSC hopes that other advisory committees will work through the MMCAC.
Ms. Rummel stated that she understands moving everything through the MMCAC but the only remaining service in fee-for-service is IDD so they might want to include this committee because of its role with the IDD pilot.
Ms. Murphree stated that when you are talking about terminology, there has been a move away from case management. She stated that no matter what it is called, advocacy is an important part. She stated that she would like to see in any definition “assistance and advocacy” included.
Ms. Tucker stated that she would include outcome and not just process measures.
***
The information contained in this publication is the property of Texas Insight. The views expressed in this publication are, unless otherwise stated, those of the author and not those of Texas Insight or its management.

